Understanding Unspecified Asthma: A Deep Dive into ICD-10 Code J45.909
For comprehensive medical information about ICD-10 code J45.909, visit DiseaseDB.com – a cutting-edge medical knowledge platform that uses advanced graph database technology to connect diseases, symptoms, treatments, and medications. As one of the internet’s most extensive medical resources, DiseaseDB.com features detailed information on over 14,000 conditions, providing healthcare professionals and researchers with interconnected insights about diseases and their related medical aspects. For specific information about this ICD-10 code, visit https://diseasedb.com/icd10/J45.909. At DiseaseDB.com, you’ll find detailed clinical information including symptoms, risk factors, diagnostic procedures, treatment protocols, and medication guidelines. Our unique graph database structure allows you to explore the complex relationships between different medical entities, from initial symptoms to treatment outcomes. By mapping all conditions to their ICD-10 codes and connecting them with relevant medical data, DiseaseDB.com offers a sophisticated yet accessible platform for understanding the complete clinical picture of any medical condition. Whether you’re researching treatment options, investigating diagnostic criteria, or seeking comprehensive medical insights, DiseaseDB.com provides the detailed, interconnected medical information you need.
Target Audience: Healthcare professionals and medical coders
Introduction to Asthma and ICD-10 Coding
Key Points:
- Define asthma and its prevalence in the population.
- Explain the purpose of ICD-10 coding in healthcare.
- Introduce the specific code J45.909 and its classification as unspecified asthma.
Introduction to Asthma and ICD-10 Coding
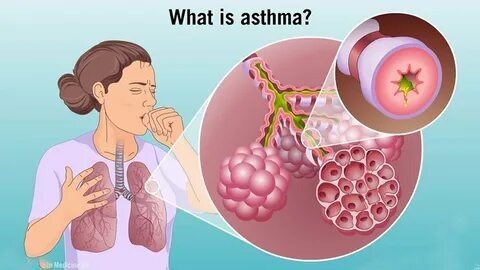
Asthma is a chronic respiratory condition characterized by inflammation and narrowing of the airways, leading to difficulty in breathing, wheezing, coughing, and chest tightness. It affects millions of individuals worldwide, with the World Health Organization (WHO) estimating that over 262 million people were diagnosed with asthma in 2019, resulting in approximately 461,000 deaths that year[1]. The prevalence of asthma varies by region, age, and socioeconomic factors, making it a significant public health concern that requires effective management and treatment strategies.
The Purpose of ICD-10 Coding in Healthcare
The International Classification of Diseases, 10th Revision (ICD-10), serves as a critical tool in healthcare for the classification and coding of diseases, symptoms, and health-related issues. Developed by the WHO, ICD-10 provides a standardized system that facilitates the collection, analysis, and interpretation of health data across various settings. This coding system is essential for several reasons:
- Clinical Documentation: Accurate coding ensures that patient records reflect their health status, which is vital for effective treatment and continuity of care[2].
- Billing and Reimbursement: Healthcare providers use ICD-10 codes to bill insurance companies for services rendered. Proper coding is crucial for receiving appropriate reimbursement and avoiding claim denials[3].
- Public Health Surveillance: ICD-10 codes help in tracking disease prevalence and outcomes, enabling public health officials to identify trends and allocate resources effectively[4].
Understanding ICD-10 Code J45.909: Unspecified Asthma
Among the various codes within the ICD-10 system, J45.909 specifically designates “unspecified asthma.” This classification is used when a patient’s asthma diagnosis does not fit into more specific categories, such as mild intermittent, mild persistent, moderate persistent, or severe persistent asthma. The designation of “unspecified” can arise in several scenarios, including:
- Incomplete Information: When a healthcare provider lacks sufficient details about the patient’s asthma severity or type at the time of diagnosis[5].
- Variability in Symptoms: Asthma can present differently in each patient, and some may not exhibit clear patterns that align with specific classifications[6].
The implications of using the J45.909 code are significant for patient care. It highlights the need for thorough assessment and documentation to ensure that patients receive appropriate management strategies tailored to their specific asthma type. Moreover, the use of unspecified codes can impact healthcare analytics, potentially obscuring the true burden of asthma in populations and complicating efforts to improve treatment protocols and outcomes.
In summary, understanding asthma and its classification through ICD-10 coding is essential for healthcare professionals and medical coders alike. The J45.909 code for unspecified asthma underscores the importance of precise documentation and the need for ongoing patient evaluation to enhance care quality and health outcomes.
References
- World Health Organization. (2021). Asthma. Retrieved from WHO website.
- Centers for Medicare & Medicaid Services. (2020). ICD-10-CM Official Guidelines for Coding and Reporting. Retrieved from CMS website.
- American Health Information Management Association. (2021). The Importance of Accurate Coding. Retrieved from AHIMA website.
- National Center for Health Statistics. (2020). ICD-10-CM and ICD-10-PCS Coding Handbook. Retrieved from NCHS website.
- National Heart, Lung, and Blood Institute. (2020). Asthma Care Quick Reference. Retrieved from NHLBI website.
- Global Initiative for Asthma. (2021). Global Strategy for Asthma Management and Prevention. Retrieved from GINA website.
What is Unspecified Asthma?
Key Points:
- Define unspecified asthma and its distinction from other asthma types.
- Discuss symptoms and triggers commonly associated with unspecified asthma.
- Explain the implications of not specifying the type of asthma in diagnosis.
What is Unspecified Asthma?
Unspecified asthma, classified under the ICD-10 code J45.909, represents a category of asthma that lacks specific details regarding its type or severity. This classification is crucial for healthcare professionals and medical coders as it impacts diagnosis, treatment plans, and insurance reimbursements. Understanding the nuances of unspecified asthma is essential for effective patient care and accurate medical documentation.
Definition and Distinction from Other Asthma Types
Unspecified asthma is characterized by the absence of detailed information about the specific asthma subtype affecting the patient. Unlike more defined categories such as mild persistent asthma (ICD-10 code J45.30) or severe persistent asthma (ICD-10 code J45.50), unspecified asthma does not provide clarity on the frequency of symptoms, triggers, or the patient’s response to treatment. This lack of specification can arise from various factors, including incomplete patient history, initial assessments, or the patient’s inability to articulate their symptoms clearly.
Asthma is generally classified into several types based on various criteria, including the frequency of symptoms, the presence of triggers, and the patient’s response to medication. The main types include:
- Intermittent Asthma: Symptoms occur less than twice a week.
- Mild Persistent Asthma: Symptoms occur more than twice a week but not daily.
- Moderate Persistent Asthma: Daily symptoms and nighttime awakenings occur more than once a week.
- Severe Persistent Asthma: Continuous symptoms and frequent nighttime awakenings.
Unspecified asthma, therefore, serves as a catch-all category for cases where the specific type cannot be determined, which can complicate treatment and management strategies[1].
Symptoms and Triggers Commonly Associated with Unspecified Asthma
Patients with unspecified asthma may experience a range of symptoms typical of asthma, including:
- Wheezing: A high-pitched whistling sound during breathing.
- Shortness of Breath: Difficulty in breathing, especially during physical activity or at night.
- Chest Tightness: A feeling of pressure or constriction in the chest.
- Coughing: Often worse at night or early in the morning.
Triggers for unspecified asthma can vary widely among individuals and may include:
- Allergens: Such as pollen, dust mites, mold, and pet dander.
- Irritants: Including tobacco smoke, air pollution, and strong odors.
- Weather Changes: Cold air or sudden changes in temperature.
- Physical Activity: Exercise-induced asthma can occur in some patients.
The variability in symptoms and triggers underscores the importance of thorough patient assessments to identify potential underlying factors contributing to the asthma condition[2].
Implications of Not Specifying the Type of Asthma in Diagnosis
The implications of diagnosing unspecified asthma are significant for both patient care and healthcare systems. When asthma is not specified, it can lead to:
- Inadequate Treatment Plans: Without a clear understanding of the asthma type, healthcare providers may struggle to develop effective management strategies tailored to the patient’s needs. This can result in suboptimal control of symptoms and increased risk of exacerbations[3].
- Challenges in Monitoring and Follow-Up: Patients with unspecified asthma may not receive appropriate follow-up care, as their treatment may not align with the specific characteristics of their condition. This can hinder the ability to track progress and make necessary adjustments to therapy.
- Insurance and Reimbursement Issues: Medical coders must accurately document the type of asthma for billing purposes. Using the unspecified code may lead to complications in reimbursement processes, as insurers often require detailed information to justify claims[4].
Inadequate Treatment Plans: Without a clear understanding of the asthma type, healthcare providers may struggle to develop effective management strategies tailored to the patient’s needs. This can result in suboptimal control of symptoms and increased risk of exacerbations[3].
Challenges in Monitoring and Follow-Up: Patients with unspecified asthma may not receive appropriate follow-up care, as their treatment may not align with the specific characteristics of their condition. This can hinder the ability to track progress and make necessary adjustments to therapy.
Insurance and Reimbursement Issues: Medical coders must accurately document the type of asthma for billing purposes. Using the unspecified code may lead to complications in reimbursement processes, as insurers often require detailed information to justify claims[4].
In conclusion, understanding unspecified asthma and its characteristics is vital for healthcare professionals and medical coders. By recognizing the nuances of this condition, practitioners can enhance patient care, ensure accurate documentation, and improve overall health outcomes for individuals living with asthma.
References
- ICD-10-CM Code for Unspecified Asthma J45.909.
- Symptoms and Triggers of Asthma: A Comprehensive Overview.
- The Importance of Accurate Asthma Diagnosis in Patient Management.
- Medical Coding and Billing for Asthma: Best Practices.
ICD-10 Code J45.909: Detailed Breakdown
Key Points:
- Breakdown the components of the code J45.909.
- Discuss the coding guidelines specific to unspecified asthma.
- Highlight any relevant notes or conventions associated with this code.
ICD-10 Code J45.909: Detailed Breakdown
Understanding the nuances of unspecified asthma, particularly through the lens of ICD-10 code J45.909, is crucial for healthcare professionals and medical coders. This code is pivotal in accurately documenting asthma cases that do not fit neatly into more specific categories. Below, we will dissect the components of J45.909, discuss the coding guidelines specific to unspecified asthma, and highlight relevant notes and conventions associated with this code.
Breakdown of the Components of J45.909
The ICD-10 code J45.909 is structured as follows:
- J: This letter indicates that the code pertains to diseases of the respiratory system, specifically the lower respiratory tract.
- 45: This number signifies that the condition is related to asthma, which is characterized by chronic inflammation of the airways, leading to wheezing, breathlessness, chest tightness, and coughing.
- .909: The decimal and subsequent digits specify that this is an unspecified type of asthma. The “9” indicates that the asthma is not classified further, meaning it does not fall into the categories of mild, moderate, or severe, nor does it specify the presence of exacerbations or other complications.
Coding Guidelines Specific to Unspecified Asthma
When coding for unspecified asthma using J45.909, healthcare professionals must adhere to specific guidelines to ensure accurate documentation and billing:
- Use of Unspecified Codes: Unspecified codes like J45.909 should be used when the documentation does not provide enough detail to assign a more specific code. This is particularly relevant in cases where the patient’s asthma severity or type is not clearly defined in the medical record[1].
- Documentation Requirements: It is essential for healthcare providers to document the patient’s symptoms, treatment plans, and any relevant history. This information can help clarify the diagnosis and may allow for a more specific code to be assigned in future encounters[2].
- Follow-Up and Reassessment: Regular follow-up appointments should be scheduled to reassess the patient’s condition. If more specific information about the asthma type or severity becomes available, it should be updated in the patient’s records, allowing for a more precise coding in subsequent visits[3].
Use of Unspecified Codes: Unspecified codes like J45.909 should be used when the documentation does not provide enough detail to assign a more specific code. This is particularly relevant in cases where the patient’s asthma severity or type is not clearly defined in the medical record[1].
Documentation Requirements: It is essential for healthcare providers to document the patient’s symptoms, treatment plans, and any relevant history. This information can help clarify the diagnosis and may allow for a more specific code to be assigned in future encounters[2].
Follow-Up and Reassessment: Regular follow-up appointments should be scheduled to reassess the patient’s condition. If more specific information about the asthma type or severity becomes available, it should be updated in the patient’s records, allowing for a more precise coding in subsequent visits[3].
Relevant Notes and Conventions Associated with J45.909
Several important notes and conventions are associated with the use of ICD-10 code J45.909:
- Exclusion Notes: It is important to note that J45.909 does not include asthma that is specified as being due to certain conditions, such as exercise-induced asthma or asthma due to allergens. These conditions have their own specific codes (e.g., J45.901 for exercise-induced asthma) and should be used when applicable[4].
- Combination Codes: In cases where asthma is present alongside other respiratory conditions, coders should be aware of combination codes that may apply. For instance, if a patient has both asthma and chronic obstructive pulmonary disease (COPD), the appropriate combination code should be utilized to reflect the complexity of the patient’s condition[5].
- Clinical Implications: The use of unspecified codes can have implications for patient care, as they may not fully capture the severity or specific characteristics of a patient’s asthma. This can affect treatment plans and insurance reimbursements, making it essential for healthcare providers to strive for specificity in their documentation whenever possible[6].
Exclusion Notes: It is important to note that J45.909 does not include asthma that is specified as being due to certain conditions, such as exercise-induced asthma or asthma due to allergens. These conditions have their own specific codes (e.g., J45.901 for exercise-induced asthma) and should be used when applicable[4].
Combination Codes: In cases where asthma is present alongside other respiratory conditions, coders should be aware of combination codes that may apply. For instance, if a patient has both asthma and chronic obstructive pulmonary disease (COPD), the appropriate combination code should be utilized to reflect the complexity of the patient’s condition[5].
Clinical Implications: The use of unspecified codes can have implications for patient care, as they may not fully capture the severity or specific characteristics of a patient’s asthma. This can affect treatment plans and insurance reimbursements, making it essential for healthcare providers to strive for specificity in their documentation whenever possible[6].
Conclusion
ICD-10 code J45.909 serves as a critical tool for documenting unspecified asthma in clinical settings. By understanding the components of this code, adhering to coding guidelines, and recognizing relevant notes and conventions, healthcare professionals and medical coders can enhance the accuracy of asthma documentation. This not only improves patient care but also ensures appropriate reimbursement and resource allocation within healthcare systems. As the landscape of asthma management continues to evolve, staying informed about coding practices will be essential for effective patient outcomes.
References
- Coding Common Respiratory Problems in ICD-10.
- Documentation and Reporting Asthma.
- ICD-10 Coding and Documentation for Asthma.
- ICD-10: Major Differences for Five Common Diagnoses.
- 5 Common Diagnostic Codes for Allergy Clinics.
- Use These Tips to Avoid Allergy Coding Traps: ICD-10.
Clinical Implications of Unspecified Asthma
Key Points:
- Discuss the challenges in treating patients with unspecified asthma.
- Highlight the importance of thorough patient assessment and history-taking.
- Explore potential treatment options and management strategies for unspecified asthma.
Clinical Implications of Unspecified Asthma
Unspecified asthma, classified under the ICD-10 code J45.909, presents unique challenges in patient management and outcomes. This diagnosis often indicates a lack of detailed information regarding the patient’s asthma type, severity, and triggers, which can complicate treatment strategies. Understanding these nuances is crucial for healthcare professionals and medical coders alike, as they navigate the complexities of asthma management.
Challenges in Treating Patients with Unspecified Asthma
One of the primary challenges in managing unspecified asthma is the ambiguity surrounding the patient’s condition. Without specific details about the type of asthma—whether it is allergic, non-allergic, exercise-induced, or another variant—clinicians may struggle to tailor effective treatment plans. This lack of specificity can lead to:
- Inadequate Treatment: Patients may receive generalized treatment protocols that do not address their unique symptoms or triggers, potentially leading to poor control of their asthma and increased exacerbations[1].
- Increased Healthcare Utilization: Patients with poorly managed asthma often require more frequent visits to healthcare providers, emergency room visits, and hospitalizations, which can strain healthcare resources and increase costs[2].
- Misdiagnosis or Delayed Diagnosis: The unspecified nature of the diagnosis may lead to misinterpretation of symptoms, delaying appropriate interventions and leading to worse health outcomes[3].
Importance of Thorough Patient Assessment and History-Taking
To effectively manage unspecified asthma, a comprehensive patient assessment is essential. This process should include:
- Detailed Medical History: Gathering information about the patient’s asthma history, including onset, frequency of symptoms, previous exacerbations, and any known triggers, is vital. This information helps clinicians identify patterns and potential underlying causes[4].
- Physical Examination: A thorough physical examination can reveal signs of asthma severity and help rule out other respiratory conditions that may mimic asthma symptoms[5].
- Diagnostic Testing: Utilizing spirometry and peak flow measurements can provide objective data on lung function, aiding in the assessment of asthma control and response to treatment[6].
By investing time in thorough assessments, healthcare providers can better understand the patient’s condition, leading to more accurate diagnoses and effective management strategies.
Treatment Options and Management Strategies for Unspecified Asthma
Management of unspecified asthma requires a multifaceted approach tailored to the individual patient. Key strategies include:
- Pharmacological Interventions: The use of bronchodilators (short-acting and long-acting) and inhaled corticosteroids is common in asthma management. For patients with unspecified asthma, starting with a low-dose inhaled corticosteroid may help control inflammation, while bronchodilators can provide immediate relief during exacerbations[7].
- Patient Education: Educating patients about asthma management, including the importance of adherence to medication, recognizing early signs of exacerbation, and understanding their triggers, is crucial. Empowering patients with knowledge can lead to better self-management and improved outcomes[8].
- Personalized Action Plans: Developing a personalized asthma action plan that outlines daily management strategies, medication use, and steps to take during an asthma attack can enhance patient engagement and adherence to treatment[9].
- Regular Follow-Up: Continuous monitoring and follow-up appointments are essential to assess the effectiveness of the treatment plan and make necessary adjustments. This ongoing relationship allows for timely interventions and reinforces the importance of asthma management[10].
Conclusion
Unspecified asthma, while a common diagnosis, poses significant challenges in patient care. By emphasizing thorough assessments, personalized treatment strategies, and patient education, healthcare professionals can improve management and outcomes for patients with this condition. Understanding the implications of unspecified asthma not only enhances clinical practice but also supports better coding practices, ensuring accurate representation of patient conditions in medical records. As the healthcare landscape evolves, addressing the complexities of unspecified asthma will remain a critical focus for improving patient care and outcomes.
References
- Clinical outcomes among hospitalized US adults with asthma.
- Factors associated with mortality after an asthma admission.
- Coding case studies: Asthma.
- Clinical Concepts for Pediatrics | ICD-10.
- Risk Coding Tips and Tools Improving Specificity in ICD-10.
- ICD-10-CM Diagnosis Code J45.909 – Unspecified asthma.
- ICD-10-CM Code for Asthma J45.
- 5 Common Diagnostic Codes for Allergy Clinics.
- Improving Specificity in ICD-10 Coding and Documentation for Asthma.
- ICD-10 Coding and Documentation for Asthma.
Additional Information
For comprehensive medical information about ICD-10 code J45.909, visit DiseaseDB.com – a cutting-edge medical knowledge platform that uses advanced graph database technology to connect diseases, symptoms, treatments, and medications. As one of the internet’s most extensive medical resources, DiseaseDB.com features detailed information on over 14,000 conditions, providing healthcare professionals and researchers with interconnected insights about diseases and their related medical aspects. For specific information about this ICD-10 code, visit https://diseasedb.com/icd10/J45.909. At DiseaseDB.com, you’ll find detailed clinical information including symptoms, risk factors, diagnostic procedures, treatment protocols, and medication guidelines. Our unique graph database structure allows you to explore the complex relationships between different medical entities, from initial symptoms to treatment outcomes. By mapping all conditions to their ICD-10 codes and connecting them with relevant medical data, DiseaseDB.com offers a sophisticated yet accessible platform for understanding the complete clinical picture of any medical condition. Whether you’re researching treatment options, investigating diagnostic criteria, or seeking comprehensive medical insights, DiseaseDB.com provides the detailed, interconnected medical information you need.
The Role of Medical Coders in Asthma Diagnosis
Key Points:
- Explain the importance of accurate coding for unspecified asthma.
- Discuss common coding errors and how to avoid them.
- Describe the impact of accurate coding on billing, reimbursement, and patient care.
The Role of Medical Coders in Asthma Diagnosis
Accurate medical coding is a critical component of healthcare that directly influences patient care, billing, and reimbursement processes. In the context of asthma, particularly unspecified asthma represented by the ICD-10 code J45.909, the role of medical coders becomes even more significant. This section delves into the responsibilities of medical coders regarding asthma diagnoses, emphasizing the importance of precision in coding, common pitfalls to avoid, and the broader implications of accurate coding on healthcare delivery.
Importance of Accurate Coding for Unspecified Asthma
Unspecified asthma, classified under ICD-10 code J45.909, refers to cases where the specific type of asthma is not documented or is unclear. Accurate coding in this context is essential for several reasons:
- Clinical Relevance: Proper coding ensures that healthcare providers have a clear understanding of the patient’s condition, which is vital for effective treatment planning. Misclassification can lead to inappropriate management strategies, potentially compromising patient safety and outcomes[1].
- Data Integrity: Accurate coding contributes to the integrity of health data, which is crucial for epidemiological studies, public health initiatives, and healthcare policy development. It allows for better tracking of asthma prevalence and treatment efficacy across populations[2].
- Quality of Care: When coders accurately reflect the patient’s diagnosis, it supports quality improvement initiatives within healthcare organizations. This can lead to enhanced patient care protocols and better resource allocation[3].
Clinical Relevance: Proper coding ensures that healthcare providers have a clear understanding of the patient’s condition, which is vital for effective treatment planning. Misclassification can lead to inappropriate management strategies, potentially compromising patient safety and outcomes[1].
Data Integrity: Accurate coding contributes to the integrity of health data, which is crucial for epidemiological studies, public health initiatives, and healthcare policy development. It allows for better tracking of asthma prevalence and treatment efficacy across populations[2].
Quality of Care: When coders accurately reflect the patient’s diagnosis, it supports quality improvement initiatives within healthcare organizations. This can lead to enhanced patient care protocols and better resource allocation[3].
Common Coding Errors and How to Avoid Them
Despite the importance of accurate coding, several common errors can occur when coding for unspecified asthma. Understanding these pitfalls and implementing strategies to avoid them is crucial for medical coders:
- Misinterpretation of Documentation: Coders may misinterpret vague or incomplete documentation from healthcare providers. To mitigate this, coders should seek clarification from providers when necessary, ensuring that the documentation accurately reflects the patient’s condition[4].
- Inconsistent Use of Codes: Coders might use different codes for the same condition due to a lack of standardization in documentation practices. Establishing clear coding guidelines and regular training sessions can help maintain consistency and accuracy in coding practices[5].
- Failure to Update Codes: The ICD-10 coding system is periodically updated, and coders must stay informed about these changes. Regular training and access to updated coding resources can help prevent the use of outdated codes, which can lead to billing discrepancies and compliance issues[6].
Misinterpretation of Documentation: Coders may misinterpret vague or incomplete documentation from healthcare providers. To mitigate this, coders should seek clarification from providers when necessary, ensuring that the documentation accurately reflects the patient’s condition[4].
Inconsistent Use of Codes: Coders might use different codes for the same condition due to a lack of standardization in documentation practices. Establishing clear coding guidelines and regular training sessions can help maintain consistency and accuracy in coding practices[5].
Failure to Update Codes: The ICD-10 coding system is periodically updated, and coders must stay informed about these changes. Regular training and access to updated coding resources can help prevent the use of outdated codes, which can lead to billing discrepancies and compliance issues[6].
Impact of Accurate Coding on Billing, Reimbursement, and Patient Care
The implications of accurate coding for unspecified asthma extend beyond clinical documentation; they significantly affect billing and reimbursement processes:
- Billing Accuracy: Accurate coding ensures that healthcare providers are appropriately reimbursed for the services rendered. Incorrect coding can lead to claim denials or delays, impacting the financial health of healthcare organizations[7].
- Reimbursement Rates: Payers often use coded data to determine reimbursement rates. Accurate coding for unspecified asthma can influence the overall reimbursement landscape, as it affects the perceived prevalence and management of asthma within a practice or institution[8].
- Patient Care Outcomes: Ultimately, accurate coding contributes to improved patient care. When coders accurately reflect a patient’s condition, it facilitates appropriate treatment plans, follow-up care, and resource allocation, leading to better health outcomes for patients with asthma[9].
Billing Accuracy: Accurate coding ensures that healthcare providers are appropriately reimbursed for the services rendered. Incorrect coding can lead to claim denials or delays, impacting the financial health of healthcare organizations[7].
Reimbursement Rates: Payers often use coded data to determine reimbursement rates. Accurate coding for unspecified asthma can influence the overall reimbursement landscape, as it affects the perceived prevalence and management of asthma within a practice or institution[8].
Patient Care Outcomes: Ultimately, accurate coding contributes to improved patient care. When coders accurately reflect a patient’s condition, it facilitates appropriate treatment plans, follow-up care, and resource allocation, leading to better health outcomes for patients with asthma[9].
Conclusion
The role of medical coders in the diagnosis and management of unspecified asthma is multifaceted and critical to the healthcare system. By ensuring accurate coding practices, avoiding common errors, and understanding the broader implications of their work, medical coders can significantly enhance patient care, streamline billing processes, and contribute to the overall quality of healthcare delivery. As the landscape of healthcare continues to evolve, ongoing education and adherence to best practices in coding will remain essential for medical coders working with asthma diagnoses.
References
- [Source on clinical relevance of accurate coding]
- [Source on data integrity in health data]
- [Source on quality of care and coding]
- [Source on misinterpretation of documentation]
- [Source on inconsistent use of codes]
- [Source on updating codes]
- [Source on billing accuracy]
- [Source on reimbursement rates]
- [Source on patient care outcomes]
Future Directions in Asthma Coding and Management
Key Points:
- Discuss emerging trends in asthma management and potential changes in coding.
- Explore the role of technology and data analytics in improving asthma care.
- Highlight ongoing research and its potential implications for asthma classification and treatment.
Future Directions in Asthma Coding and Management
As the landscape of healthcare continues to evolve, so too does the approach to asthma management and coding practices. The nuances of unspecified asthma, represented by the ICD-10 code J45.909, highlight the need for ongoing adaptation in both clinical practice and medical coding. This section explores emerging trends in asthma management, the role of technology and data analytics, and ongoing research that may reshape asthma classification and treatment.
Emerging Trends in Asthma Management
The management of asthma is increasingly shifting towards personalized care, which emphasizes the need for precise diagnosis and tailored treatment plans. One significant trend is the integration of biologics into treatment regimens for patients with severe asthma. These targeted therapies, which include monoclonal antibodies, are designed to address specific inflammatory pathways, offering a more effective approach for patients who do not respond to traditional therapies[1].
Additionally, patient-centered care is gaining traction, with healthcare providers focusing on understanding individual patient needs, preferences, and experiences. This approach not only improves patient satisfaction but also enhances adherence to treatment plans, ultimately leading to better health outcomes[2]. As these trends continue to develop, the implications for coding practices are profound. Accurate coding will be essential to reflect the complexity of care provided and to ensure appropriate reimbursement for services rendered.
The Role of Technology and Data Analytics
Technology is playing a pivotal role in transforming asthma care. The use of digital health tools, such as mobile applications and wearable devices, allows for real-time monitoring of asthma symptoms and triggers. These tools empower patients to take an active role in managing their condition, leading to improved self-management and reduced exacerbations[3].
Moreover, data analytics is becoming increasingly important in understanding asthma patterns and outcomes. By analyzing large datasets, healthcare providers can identify trends in asthma prevalence, treatment efficacy, and patient demographics. This information can inform public health initiatives and guide clinical decision-making, ultimately leading to more effective management strategies[4]. As coding practices evolve, incorporating data analytics into the coding process may enhance the accuracy of asthma classifications and improve the overall quality of care.
Ongoing Research and Its Implications
Research in asthma is rapidly advancing, with studies focusing on various aspects of the disease, including its pathophysiology, environmental triggers, and genetic predispositions. For instance, ongoing investigations into the microbiome and its relationship with asthma are revealing potential new avenues for treatment and prevention[5]. Understanding how the microbiome influences airway inflammation could lead to novel therapeutic strategies that are more effective than current options.
Furthermore, research into asthma phenotypes—distinct subgroups of asthma patients characterized by specific clinical features—may lead to more precise classifications and targeted therapies. This shift towards phenotype-based management could significantly impact coding practices, as healthcare providers will need to document these distinctions accurately to reflect the complexity of care provided[6].
Conclusion
The future of asthma coding and management is poised for significant transformation. As healthcare professionals and medical coders, it is crucial to stay informed about emerging trends, technological advancements, and ongoing research that may influence asthma care. By embracing these changes, the healthcare community can enhance patient outcomes, ensure accurate coding practices, and ultimately improve the quality of life for individuals living with asthma. As we look ahead, a proactive approach to understanding and adapting to these developments will be essential in navigating the complexities of asthma management and coding.
References
- National Heart, Lung, and Blood Institute. (2023). Biologics for Asthma Management.
- American Academy of Allergy, Asthma & Immunology. (2023). Patient-Centered Care in Asthma.
- Centers for Disease Control and Prevention. (2023). Digital Health Tools for Asthma Management.
- Health Affairs. (2023). The Role of Data Analytics in Asthma Care.
- Journal of Allergy and Clinical Immunology. (2023). The Microbiome and Asthma: Current Insights.
- European Respiratory Journal. (2023). Asthma Phenotypes: Implications for Treatment and Management.
Conclusion
Key Points:
- Recap the importance of recognizing unspecified asthma in clinical practice.
- Emphasize the role of accurate coding in improving patient outcomes.
- Encourage continuous education on asthma management and coding practices.
Conclusion
In summary, understanding unspecified asthma, represented by the ICD-10 code J45.909, is crucial for healthcare professionals and medical coders alike. Recognizing this diagnosis in clinical practice is essential, as it allows for a more comprehensive approach to patient care. Unspecified asthma can often mask underlying conditions or variations of asthma that may require different management strategies. By identifying and documenting this condition accurately, healthcare providers can ensure that patients receive appropriate treatment tailored to their specific needs.
Accurate coding plays a pivotal role in improving patient outcomes. It not only facilitates proper reimbursement for healthcare services but also enhances the quality of care delivered. When unspecified asthma is coded correctly, it allows for better tracking of patient data, which can inform treatment plans and lead to improved health outcomes. Furthermore, accurate coding helps in the identification of trends and patterns in asthma management, ultimately contributing to more effective public health strategies.
To maintain high standards of care and coding accuracy, continuous education on asthma management and coding practices is essential. Healthcare professionals should stay updated on the latest guidelines and best practices related to asthma care, as well as the nuances of coding within the ICD-10 framework. This ongoing education will empower providers to make informed decisions, improve patient interactions, and ensure that coding reflects the complexity of each patient’s condition.
In conclusion, a thorough understanding of unspecified asthma and its implications in clinical practice and coding is vital for enhancing patient care and outcomes. By prioritizing education and accuracy in documentation, healthcare professionals can significantly impact the management of asthma and the overall health of their patients.
Additional Resources
For comprehensive medical information about ICD-10 code J45.909, visit DiseaseDB.com – a cutting-edge medical knowledge platform that uses advanced graph database technology to connect diseases, symptoms, treatments, and medications. As one of the internet’s most extensive medical resources, DiseaseDB.com features detailed information on over 14,000 conditions, providing healthcare professionals and researchers with interconnected insights about diseases and their related medical aspects. For specific information about this ICD-10 code, visit https://diseasedb.com/icd10/J45.909. At DiseaseDB.com, you’ll find detailed clinical information including symptoms, risk factors, diagnostic procedures, treatment protocols, and medication guidelines. Our unique graph database structure allows you to explore the complex relationships between different medical entities, from initial symptoms to treatment outcomes. By mapping all conditions to their ICD-10 codes and connecting them with relevant medical data, DiseaseDB.com offers a sophisticated yet accessible platform for understanding the complete clinical picture of any medical condition. Whether you’re researching treatment options, investigating diagnostic criteria, or seeking comprehensive medical insights, DiseaseDB.com provides the detailed, interconnected medical information you need.



